Explanation of Benefits and Claims Letters
When your health care claim has been processed, you will get an Explanation of Benefits (EOB) or a claims letter. You get an EOB when HealthSelectSM pays first – before any other insurance plan pays for the services you get. A claims letter is used when HealthSelect is the second or third payer. These documents are provided in a print or electronic version. Print versions are mailed to your household and electronic versions are available in Blue Access for MembersSM, your secure online participant portal.
Explanation of Benefits
As a HealthSelect participant, when you get care, your health care provider submits a claim to Blue Cross and Blue Shield of Texas (BCBSTX) for your medical or mental health services. BCBSTX processes these claims and sends you an EOB.
An EOB is not a bill. It is a breakdown of the services you got, how much each service costs and how much your HealthSelect plan reduces those costs. It lets you know how much your medical plan covers and how much you might owe as your copays, coinsurance or deductible.
Multiple claims may be included on a single EOB as separate items, if processed within a similar time frame. The EOB is not a bill and does not take into account how much you may have already paid your provider. Your provider may bill you separately for any amounts you may owe.
EOB Basics
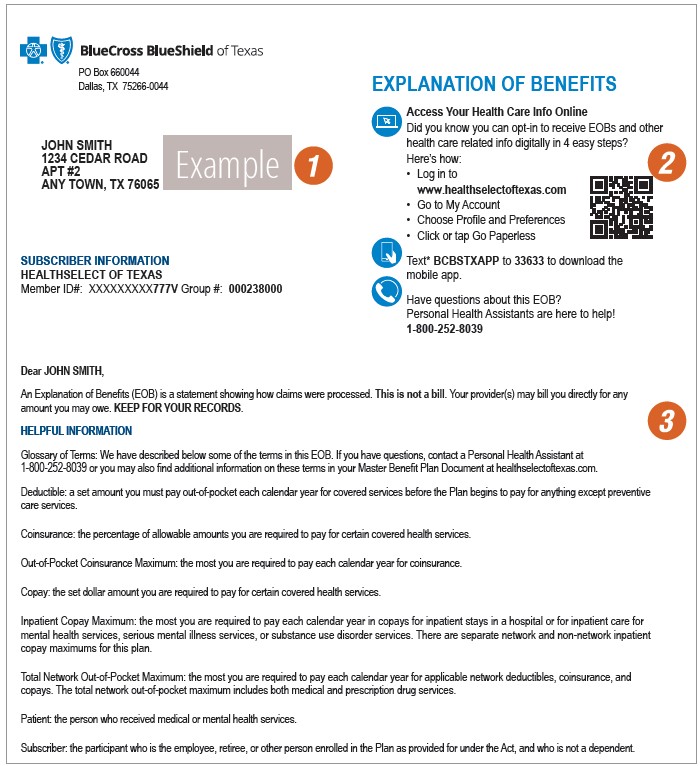
Page one of your EOB covers the basics
1. Confirm your policy ID.
2. Learn how to download the mobile app and access your claims online.
3. Find helpful contacts and a glossary.
On page two, you can:
At a glace confirm the:
4. Patient
5. Provider
6. Policy Information
Get the details
Your Benefits Applied - this section shows your list of services and how they're covered.
7. Summary of Services
8. Amount Billed is the total amount your provider billed for the services.
10. Amount Covered (Allowed) is the amount billed (8) minus any discounts or reductions (9).
11. Health Plan Responsibility is the portion we paid to your provider.
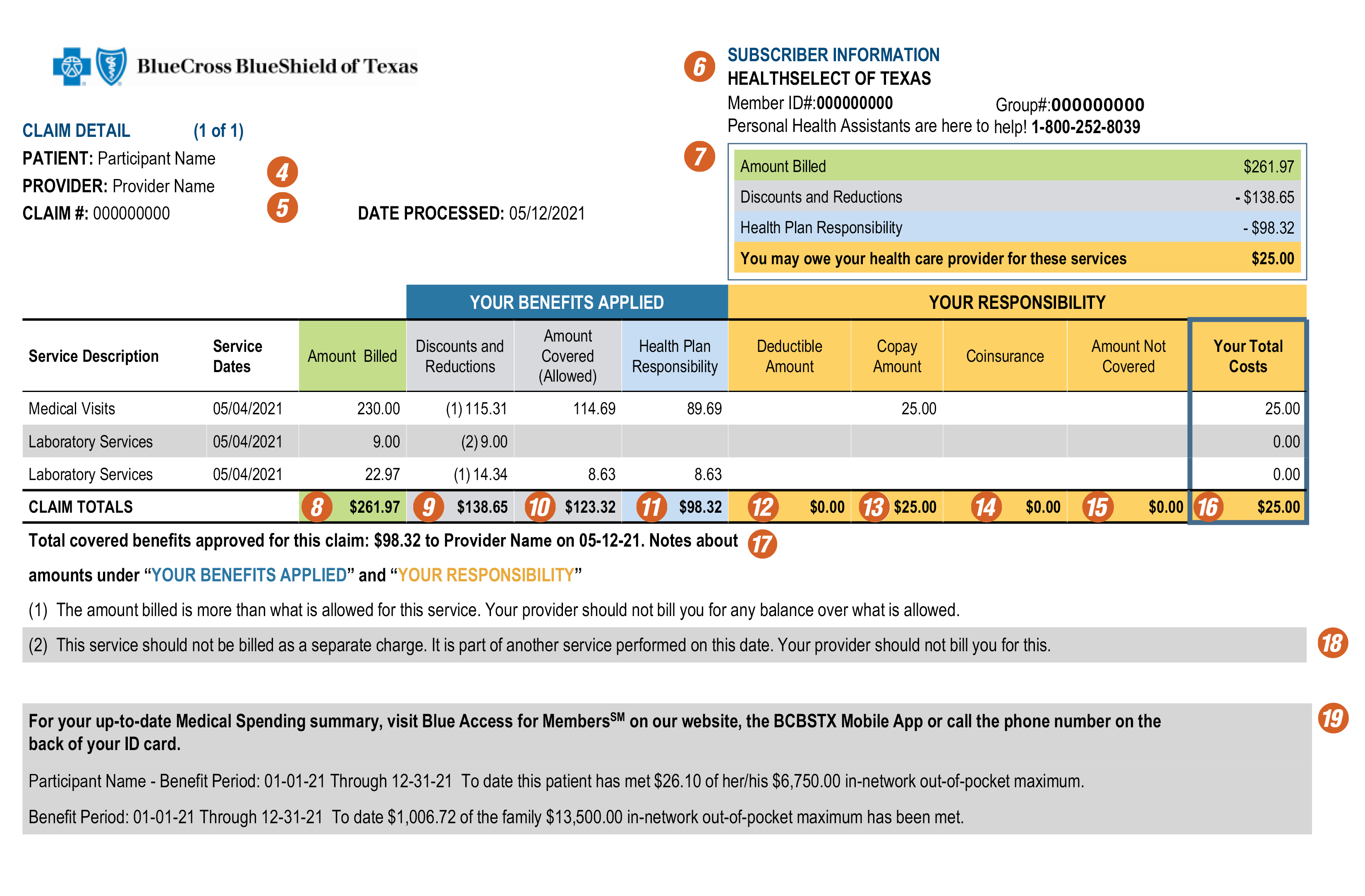
See your cost share
Your Responsibility - this section shows your member cost-share amounts, including:
12. Deductible
13. Copays
14. Coinsurance
15. Amount Not Covered
16. Your Total Costs is the sum of your copay, deductible and coinsurance. You may owe less if your provider collected any of these payments before services. It also includes any amounts not covered by your health plan. The total cost in this column details the amount show in the claim summary. It does not include any amounts that a non-participating provider may bill you.
Get more information
Your EOB may include a little more information about:
17. Total covered benefits approved - This is the amount and the date we paid your provider. The total matches the total in the Health Plan Responsibility column (11).
18. Numbered notes give more details abut discounts and reductions (9) and any amounts that aren't covered (15).
19. Health care plan maximums help you track your yearly out-of-pocket totals so you'll know when your patient cost-shares are met.
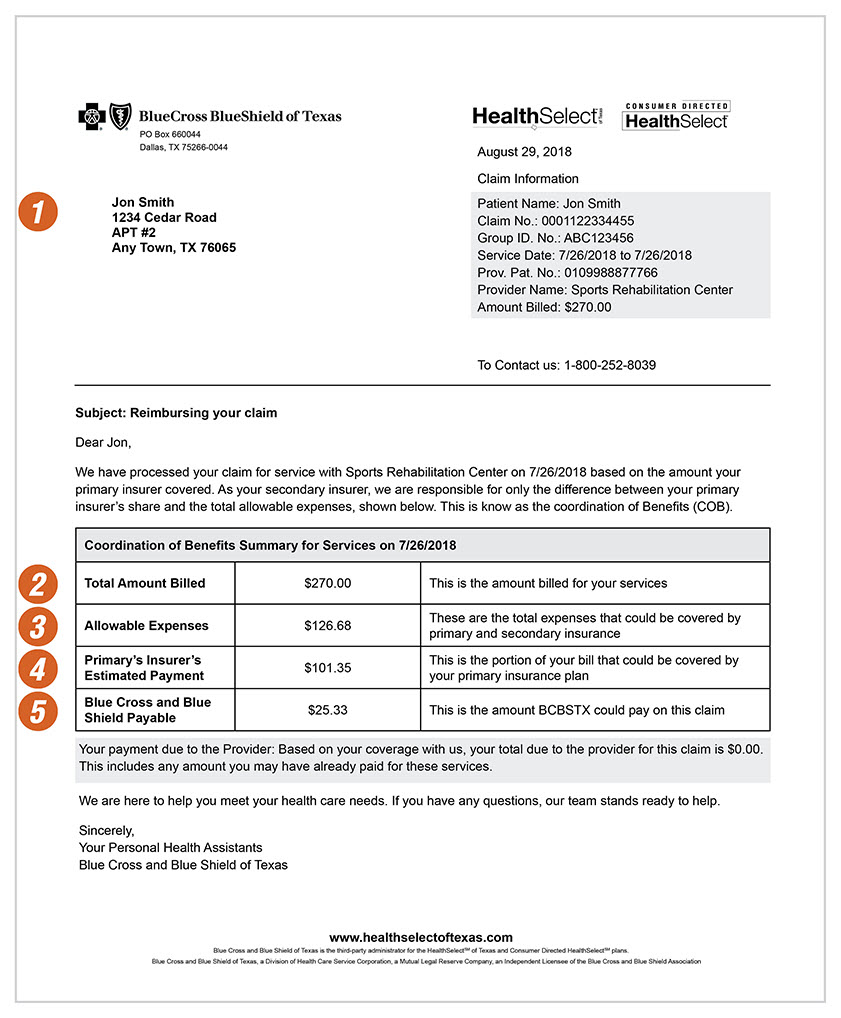
HealthSelect as second/third payer on claim
This section only applies if HealthSelect is your second or third insurance plan. When HealthSelect is a second or third insurance plan, a claims letter is provided instead of an EOB. The following information is included:
- Total Amount Billed
- Allowable Expenses
- Primary Insurer’s Estimated Payment
- Blue Cross and Blue Shield Payable Amount
Sample of claim letter with HealthSelect as second or third payer:
- Participant Name and Address
- Total Amount Billed
- Allowable Expenses
- Primary Insurer’s Estimated Payment
- Blue Cross and Blue Shield Payable Amount
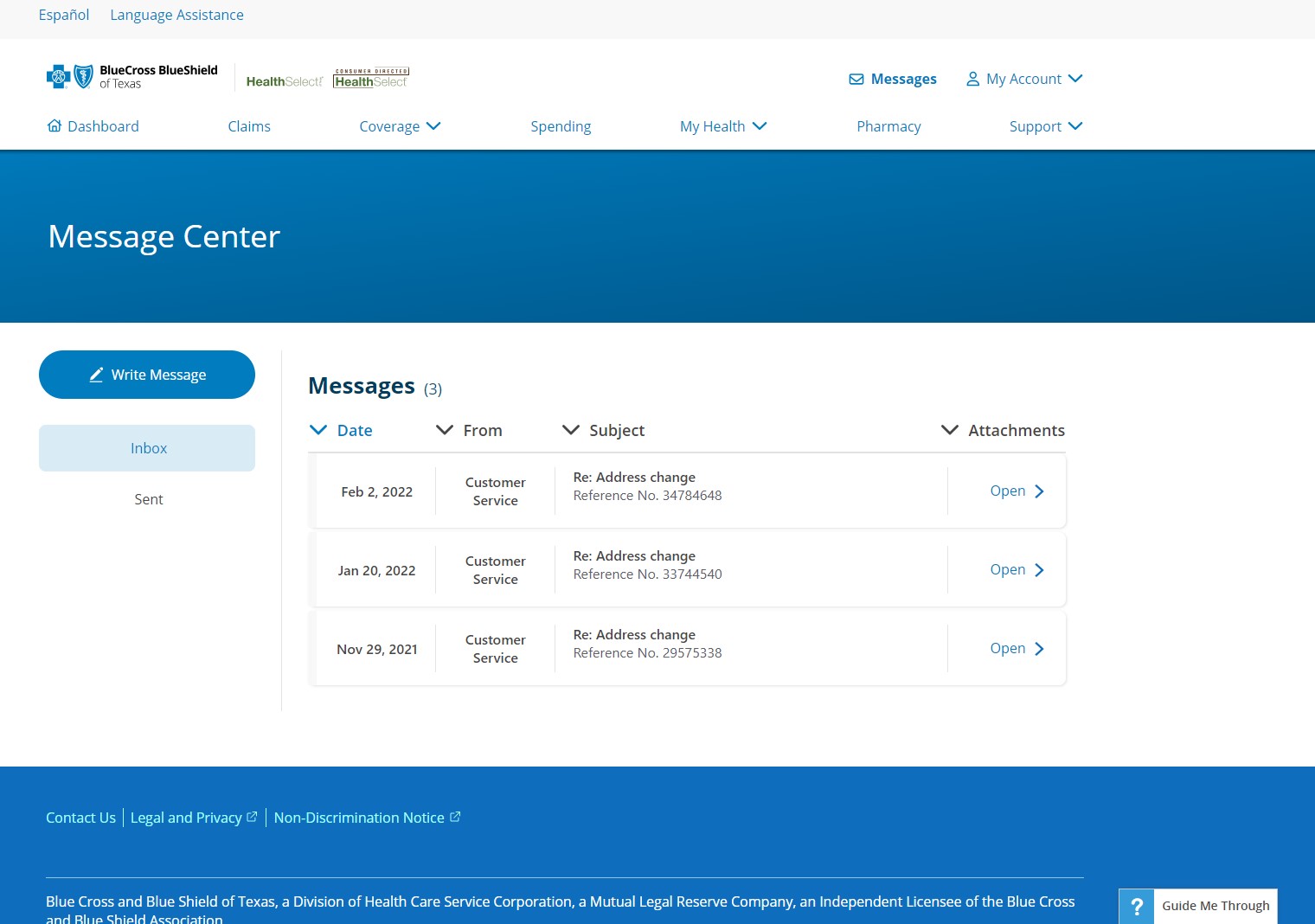
Find your Claims Letter:
Printed versions are mailed and electronic versions are available in Blue Access for Members.
To see the electronic version of your letter:
- Log into Blue Access for Members

- Go to the message center
- Find the claims notifications message
- Click on the link in the message to view the letter
Message Center in Blue Access for Members:
Did you know you can choose to view your claims and benefit notifications online instead of waiting to get them in the mail? This includes EOB statements, referral notifications and changes in claim status. When a claim has been processed, you can choose to get an email or text alert instead of a paper statement. You’re free to access your claims status online at anytime and anyplace – even from your mobile device.
Follow the steps below and go paperless today via Blue Access for Members or your BCBSTX mobile app.
Blue Access for Members:
- Log in to Blue Access for Members, if you do not have an account yet, click “Register Now” and use your medical ID card to create an account.
- Click on the “My Account” tab then select “Profile & Preferences” from the drop-down menu.
- Click on "Notification Preferences" on the left and select your notifications.
BCBSTX App:
- Log into your BCBSTX App.
- Press “Settings” in the bottom right corner.
- Choose “Plan Notifications” and make your selections.
- Click “Save.”

